I AM Nearing Retirement
Retirement is a big step. Take the uncertainty out of it by ensuring that you are prepared.
Show me More


I AM A New Member
Just retired? Learn more about your benefits and what to expect as a new Trust member.
Show me More


I AM Interested in Medicare
Getting closer to age 65? Let us help you make sense of Medicare and how your Trust benefits work.
Show me More


Information For You
Get the latest news and updates from the Trust
Video: Enhanced 2024 Trust OTC Benefit
Watch a short video to learn more about the 2024 Trust OTC benefit changes.
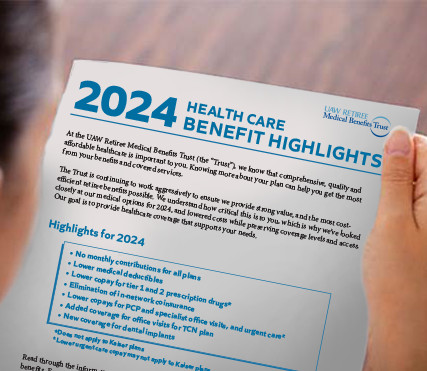
Video: Learn about your 2024 benefits
Watch a recently recorded webinar to learn more about your 2024 Trust benefits.
Health & Wellness
Everything you need at your fingertips to stay happy and healthy
Winter Travel Tip: Use a Medical Checklist
Traveling this winter? Be sure to have a medical checklist. It can help prepare you in the case of a medical emergency. Learn how to create yours before you travel this season.
Learn More